19A127
A Quality Improvement Intervention to Increase Pnuemococcal and Influenza Vaccination Amongst Immunosuppressed Inflammatory Arthritis Patients
Author(s)
K Murray, C Lowe, A O’Rourke, F Young, I Callanan, E Feeney, D Veale
Department(s)/Institutions
Saint Vincent’s University Hospital
Introduction
CDC guidelines recommend influenza and 23-valent pneumococcal polysaccharide (PPSV23) vaccination for inflammatory arthritis (IA) patients on immunosuppression.
Aims/Background
This study aimed to:
1). assess barriers to vaccination
2). increase PPSV23 (5 yearly) and “flu” (annual) vaccination uptake in immunosuppressed IA outpatients through a multifaceted quality improvement (QI) intervention. The primary outcome was adequate PPSV23 and “flu” vaccination of immunosuppressed IA outpatients.
Method
Consecutive outpatients from 2017 were invited to complete an anonymous 23 question paper questionnaire including demographic, diagnostic, medication and vaccination (knowledge, status and barriers) data. Patients taking oral steroids, biologic DMARDs (bDMARDs) or immunosuppressant conventional synthetic agents (csDMARDs) were included.
Simultaneously, a low cost multifaceted QI intervention was performed. This involved staff education sessions, patient information questionnaires, point-of-care paper “Arthritis and Infection Worksheets” and “Vaccination Advice Letters” highlighting outstanding vaccinations to the patient’s GP. In 2018, post-intervention, the clinic was re-assessed. Binary logistic regression analysis was used to assess for independent predictors of up-to-date vaccination.
Results
In 2017-2018, 163 and 262 patients, respectively, met inclusion criteria. Patients were typical of an IA clinic (74% women; 45.4% ≥60 years old; 72.7% RA; 61.1% using csDMARDs; 46.6% using bDMARDs; 23.1% using combination csDMARD plus bDMARD; 32.5% using oral steroids).
In 2017, 104 (65.4%) knew of the increased infectious risk with IA. In 2018, 168 (65.6%) were aware. In 2017, 111 (69.8%) were aware of increased infection risk with medications;172 (66.9%) in 2018.
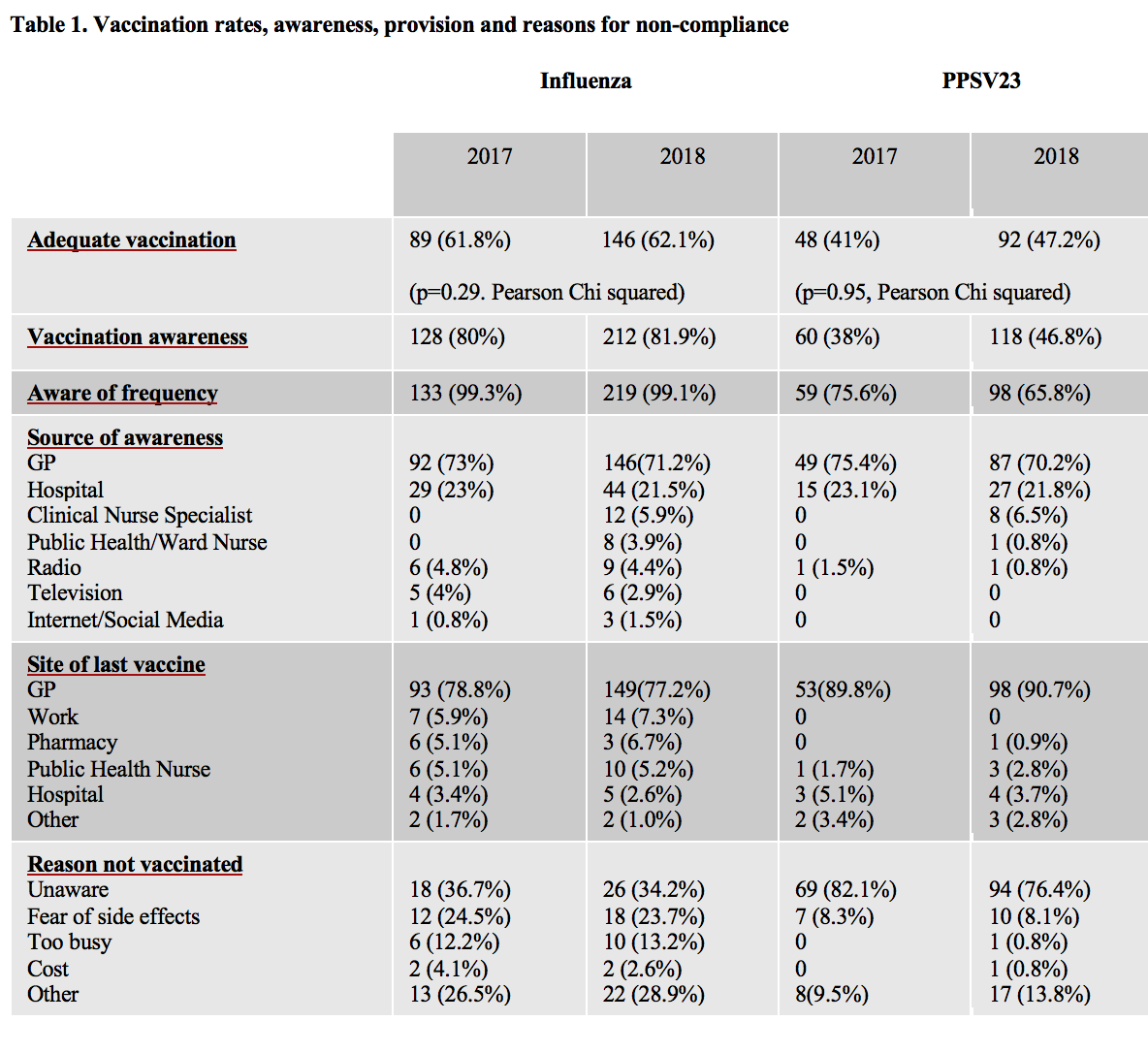
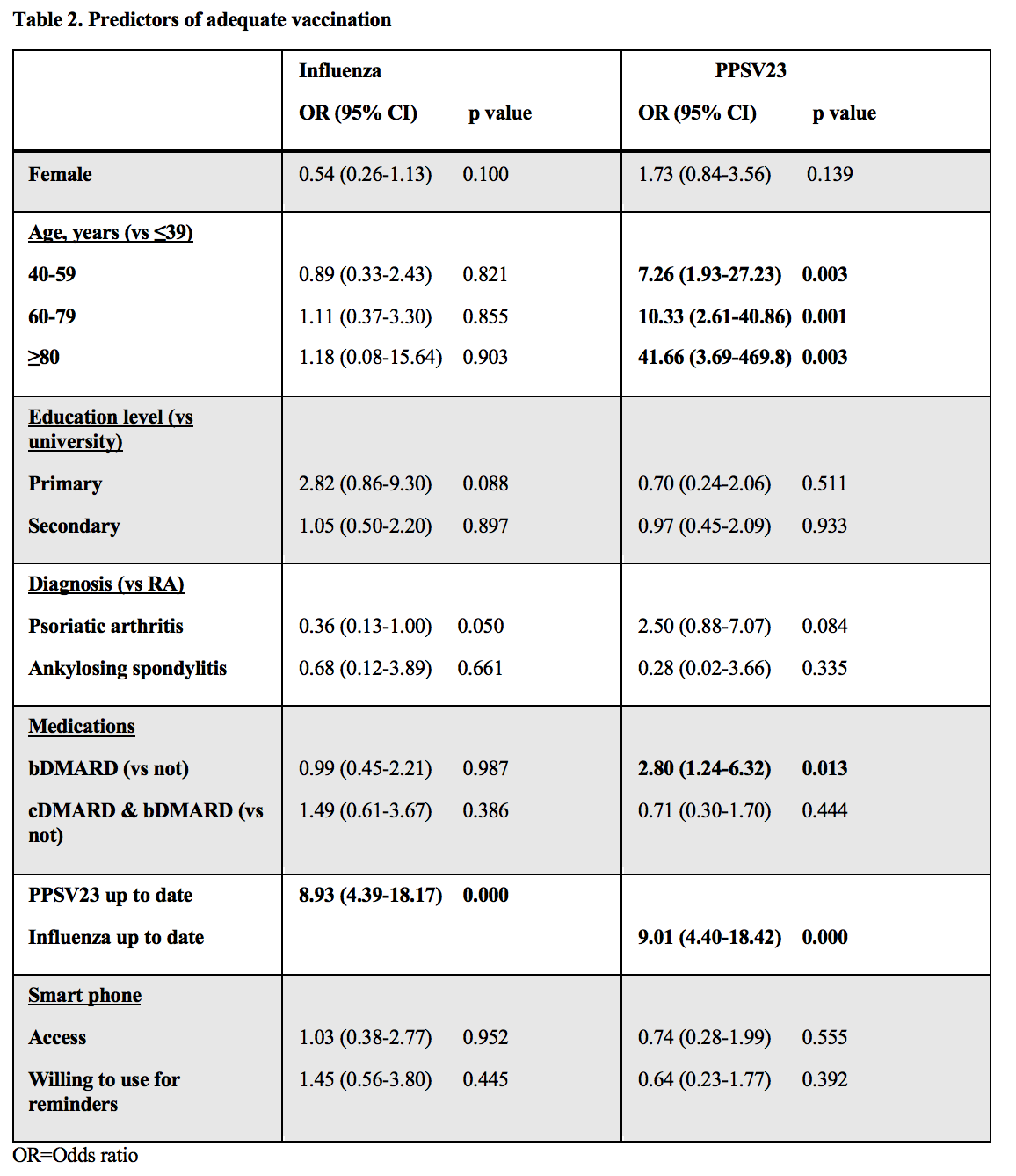
Vaccination rates and awareness were higher for “flu” (Table 1). GPs informed and vaccinated most patients. The most common reason for non-vaccination was lack of awareness. 70% of patients had smart phone access. 78% were willing to use this for vaccination reminders. Age, bDMARD use and up-to-date influenza vaccination were significant predictors of PPSV23 vaccination (Table 2). Only, up-to-date PPSV23 vaccination predicted “flu” vaccination.
Conclusions
Influenza and PPSV23 vaccination rates were suboptimal and increased marginally. One potential solution is point-of-care vaccination in clinic. We have applied for funding for this. Currently, <5% of vaccinations are in hospital. Specialists sharing responsibility with GPs may optimise vaccination timing, safety and uptake.